The Anatomy of an Ear Infection - Risks, Symptoms, and Treatments




DOES YOUR CHILD HAVE AN EAR INFECTION? HOW TO TELL.
Your child has a bothersome cold for a week. Her nasal discharge turns a little green and her cough starts to keep you all up at night. Then one night she is up every hour extremely fussy with a fever. You take her into the doctor in the morning almost certain she has another ear infection.
Ear infections are one of the most worrisome illnesses for both parents and children to go through, especially if they frequently recur. They also are the most common reason for antibiotic prescriptions. Here's a guide to help you understand why ear infections occur, how to best treat them, and most importantly, how you can prevent them from happening too often.
EIGHT MAIN SYMPTOMS OF AN EAR INFECTION
Your child may have 2 or more of these symptoms:
- Cold symptoms – keep in mind that ear infections are almost always preceded by a cold. Often a clear runny nose will turn yellow or green before an ear infection sets in.
- Fussiness during the day or night
- Complaining of ear pain or hearing loss
- Night-waking more frequently
- Unwillingness to lie flat
- Fever – usually low grade (101º - 102º); may not have a fever.
- Sudden increase in fussiness during a cold
- Ear drainage – if you see blood or pus draining out of the ear, then it is probably an infection with a ruptured eardrum. DON'T WORRY! These almost always heal just fine, and once the eardrum ruptures the pain subsides.
YOUR CHILD IS UNLIKELY TO HAVE AN EAR INFECTION IF:
1. No cold symptoms – if your child has some of the above symptoms but does not have a cold, an ear infection is less likely, unless your child has had an ear infection in the past without a cold.
2. Pulling at the ears or batting the ears in infants less than 1 year of age. Infants less than one are unable to precisely localize their ear pain. This means that they cannot tell that the pain is coming from the ear or from structures near the ear. Infants can pull on or bat at their ears for two other common reasons:
- Teething – Baby thinks the pain from sore gums is coming from the ears
- Because they like playing with their ears – Infants are fascinated with these strange appendages that are sticking out of the side of their head. They love to explore them, play with them, and especially to stick their finger into that strange hole in the middle.
3. No complaints of ear pain in a child who is old enough to tell you, usually by age two or three.
HOW CAN I TELL IF IT'S AN EAR INFECTION OR JUST TEETHING?
Are you tired of taking your fussy baby into the doctor just to check her ears, only to be told its probably just teething? TO help you decide, with teething:
- Pain usually starts at four months of age and will come and go until the two-year molars are in.
- Tugging or digging at the ears with no cold symptoms or fever
- Fussiness or night waking with no cold symptoms or fever
- May have low fever less than 101
- Teething does not cause a runny nose, only drool.
HOW DO EAR INFECTIONS OCCUR
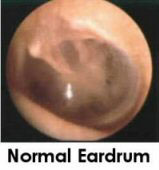
Anatomy lesson. The ear is divided into three parts: the outer ear canal, the middle ear space where infections occur, and the inner ear where the nerves and balance center are. A thin, membranous eardrum divides the outer and middle ear. The middle ear space is also connected to the back of the nose via the Eustachian tube.
Immature Eustachian tube. In infants and young children this tube is much shorter and is angled. It is therefore much easier for bacteria to migrate from the nose and throat up into the middle ear space. As the child grows this tube becomes more vertical, so germs have to travel "up hill" to reach the middle ear. This is one-reason children "outgrow" ear infections.
Colds. When your child has a cold, the nasal passages get swollen and mucus collects in the back of the nose. This environment is a breeding ground for the bacteria that normally live in the nose and throat to begin to overgrow. Mucus is also secreted within the middle ear space just as it is in the sinuses.
Bacterial invasion. Germs migrate up through the Eustachian tube and into the middle ear space where they multiply within the mucus that is stuck there. Pus begins to form and soon the middle ear space is filled with bacteria, pus and thick mucus.
Ear pain. This pus causes the eardrum to bulge causing pain. It is this red, bulging pus-colored eardrum that the doctor can see by looking into the ear canal.
Diminished hearing. The discharge that collects in the middle presses on the eardrum preventing it from vibrating normally. This is what the doctor means by "fluid in the middle ear." Also the fluid plugs the eustachian tube and dampens the sound like the sensation in your ears during air travel.
ARE EAR INFECTIONS CONTAGIOUS?
No, the bacteria inside the ear causing the infection are not contagious. The cold virus that can lead to an ear infection is contagious. Oftentimes, if the ear infection occurs a week after the cold begins, the child is no longer contagious.HOW ARE EAR INFECTIONS TREATED?
- Acetaminophen or ibuprofen are effective pain relievers for ear pain. You can safely use both medications together if one alone is not enough. Click on each medication for dosage.
- Warm compress – apply a warm washcloth to the ear.
- Warm olive oil, vegetable oil, or garlic oil – put several drops of one of these into the ear. MAKE SURE THE OIL ISN’T TOO HOT.
- Anesthetic eardrops – if the above remedies aren’t enough, these are available by prescription and can numb the eardrum to minimize the pain for an hour or two.
- WARNING – if you see any liquid or pus draining out of the ear, DO NOT PUT ANY OF THE ABOVE DROPS INTO THE EAR. See below under ear drainage.
- Amoxicillin – "the pink stuff" – this is the standard first-line treatment used by most doctors, and rightly so. It works well most of the time, is inexpensive, tastes pretty good, and is easy on the stomach and intestines.
- Azithromycin, Augmentin (amoxicillin/clavulinate mix), double dose amoxicillin, cefuroxime – this are all common second and third line choices.
- A new combination of Augmentin plus extra amoxicillin called Augmentin ES has been shown to be very effective in treating resistant ear infections. Your doctor may prescribe both.
- Finish the prescribed course – even if you child is feeling better after two or three days, it is best to complete at least seven days of treatment to help ensure the infection doesn't come back.
Avoid antibiotic resistance - But doctor, amoxicillin doesn't work for my child, and it's so hard to give it to her three times a day! Can I please have the once a day for only five days stuff? Be careful about doing this. Always taking a stronger, more convenient antibiotic can make the bacteria that dwell in your child more resistant to the stronger antibiotics, and can make future infections more difficult to treat. Even if amoxicillin hasn't worked once or twice in the past, chances are that this new infection is a different bacteria that is sensitive to amoxicillin, especially if more than two months have passed since the last antibiotic. The good news is amoxicillin now comes in a twice-a-day form, and treatment is usually only seven days, not ten.
- If the fever and fussiness are not improving after 48 – 72 hours of an antibiotic, your child may need a stronger one.
- If amoxicillin has not worked two or three times in the past, then it's ok to start with a stronger antibiotic for future infections.
- If your child has taken amoxicillin in the past six weeks, and then develops another ear infection, chances are that this infection is resistant and needs a stronger antibiotic.
- If your child is allergic to amoxicillin
- If the infection is still present after one course of amoxicillin
- Important note – the antibiotics only take care of the bacteria causing the ear infection. They don't treat the virus that is causing the underlying cold symptoms. So don't expect the runny nose and cough to improve for 3 to 14 days.
ARE ANTIBIOTICS ABSOLUTELY NECESSARY TO TREAT EAR INFECTIONS?
No, they are not absolutely necessary, but they are very helpful for several reasons:
- Antibiotics will help your child feel better faster by eliminating the bacteria, which in turn reduces the fever and ear pain more quickly. Children generally feel better after one or two days of antibiotics.
- Allowing an ear infection to heal on its own usually subjects a child to four to seven days of fever and ear pain.
- Antibiotics help prevent the very rare, but possible, complications of an ear infection spreading into the brain or bone surrounding the ear.
- New research is suggesting that 80% of uncomplicated ear infections will resolve within 4 to 7 days without antibiotics. Parents who choose not to use antibiotics can treat the pain and fever with Auralgan anesthetic ear drops and ibuprofen or acetominophen.
MINIMIZING THE SIDE EFFECTS OF ANTIBIOTICS
Side effects can include:
- Diarrhea
- Fungal diaper rash
- Oral thrush
- Vomiting
- Rash
HOW EAR INFECTIONS RESOLVE
There are two components of ear infections that need to resolve:
- Infection – the antibiotics usually take care of the bacteria, which in turn resolves the fever and pain with a few days.
- Middle ear fluid – it takes much longer for this to resolve, anywhere from a few days up to 3 months! The fluid slowly drains out through the Eustachian tube down into the nose. Taking repeated courses of antibiotics does not speed up this process, since the fluid is usually no longer infected with bacteria. Chronic nasal congestion or allergies can block the Eustachian tube and therefore prevent the ears from draining. Your child's hearing may be muffled until the fluid drains out. This is not permanent. See below on preventing ear infections for tips on how to improve ear drainage.
- Remember, since the runny nose and cough are usually caused by a cold virus and not bacteria, it may be 3 – 14 days before these symptoms resolve.
FOLLOW UP WITH THE DOCTOR
Most doctors will have you follow up anywhere from one to four weeks after an ear infection. There are several reasons for this:
- To make sure the infection is clearing up
- To make sure the middle ear fluid is draining out. If the fluid stays around continuously for more than three months, your doctor needs to know.
- To help determine if the next ear infection is a new one or a continuation of an old infection. This helps determine which antibiotic to use.Your doctor may perform a tympanogram – a rubber probe that painlessly fits into your baby's ear canal and measures how the eardrum vibrates. This helps determine if there is any fluid left.
IMPORTANT NOTE: Try to avoid over-treating with unnecessary repeated courses of antibiotics. At your follow-up visit with your doctor, there may still be fluid in the middle ear. If the ear is not red or bulging, and your child is acting fine, you may not need another course of antibiotics. Doctors will vary in how aggressive they like to treat ear fluid. You may be able to spare your child from an unnecessary course of antibiotics.
CHRONIC EAR FLUID
As stated above, sometimes it can take several months for the fluid to drain out of the middle ear space. During this period the hearing can be muffled. This isn't dangerous and does not cause permanent hearing loss. Thankfully, the fluid often drains out within two or three weeks. There are several situations, however, when you do need to worry about this fluid in the ear:
- Eustachian tube dysfunction – this is a condition where the Eustachian tube can't do its job correctly and the middle ear doesn't drain. Causes include chronic sinus infections, nasal allergies and frequent colds.
- Fluid that stays in the ear for more than three to four months can become thick and gooey, a term called "glue ear". This type of fluid often needs to be drained surgically by an ear specialist.
- If this long period of muffled hearing occurs during the first two years of life when language development is crucial, it can cause speech delay. This is usually only temporary, however, but the longer it goes on, the longer the speech and hearing can be delayed.
- If your child has several ear infections over a three to four month period, and the fluid never really has time to drain in between infections, this can cause a prolonged period of muffled hearing.Again, don't worry if it takes one or two months for the fluid to drain out of your child's ear. This is common. We would like to stress, however, the importance of proper follow-up with your doctor to make sure it eventually resolves.
NINE STEPS TO PREVENTING EAR INFECTIONS
If your child has had several ear infections already, or you simple wish to lower her risk of getting them in the first place, here are some ways to prevent or at least lessen the frequency and severity of ear infections:
1. Breastfeeding. There is no doubt whatsoever in the medical literature that prolonged breastfeeding lowers your child's chances of getting ear infections.
2. Daycare setting. Continuous exposure to other children increases the risk that your child will catch more colds, and consequently more ear infections. Crowded daycare settings are a set up for germ sharing. If possible, switch your child to a small, home daycare setting. This will lower the risk.
3. Control allergies.
4. Feed baby upright. Lying down while bottle-feeding can cause the milk to irritate the Eustachian tube which can contribute to ear infections.
5. Keep the nose clear. When a runny nose and cold start, do your best to keep the nose clear by using steam, saline nose drops, and suctioning. See colds for more info on this.
6. Cigarette smoke. There is strong evidence that smoking irritates baby's nasal passage, which leads to Eustachian tube dysfunction.
8. Eat more raw fruits and vegetables - these can greatly boost your child's immune system and help fight off infections.
MEDICAL PREVENTION FOR CHRONIC OR FREQUENT EAR INFECTIONS
If your child is having frequent ear infections, more aggressive prevention may be indicated. There are different opinions as to the definition of chronic ear infections. How many is too many?
- More aggressive doctors may choose to begin medical prevention if you child has more than three ear infections in six months, or more than four in one year.
- Less aggressive doctors may allow your child to have more infections before recommending medical prevention. We lean more in this direction.
- Other factors such as hearing loss and speech delay may warrant more aggressive treatment.
There are three forms of medical prevention:
- Prophylactic antibiotics. This consists
of a once-a-day dose of amoxicillin or similar
antibiotic. There are two ways to do this:
- Daily treatment for several months continuously, such as through the winter season.
- Start the daily treatment at the first sign
of any cold symptoms, and then continue the
antibiotic for 7 – 10 days.
- Advantage to taking prophylactic antibiotics is that you avoid full dose courses of possibly stronger antibiotics.
- Disadvantage is that your child gets and antibiotic possibly more often and this could contribute to antibiotic resistance.
- OUR PREFERENCE is to start the daily amoxicillin at the first sign of cold symptoms.
- Immunization. There is a new vaccine
called Prevnar that came out in 2000. Four doses are
given during the first two years of life. For
children 15 months and older, one dose is enough.
This vaccine helps prevent infections from a
bacterium called pneumococcus. This bug causes
pneumonia, blood infections, meningitis and ear
infections. The main purpose of this vaccine is to
prevent the more serious infections. It also can
prevent ear infections in two ways:
- Decreased number of ear infections – this effect is minimal. Studies have shown that this shot only decreases ear infections by 10 – 20%.
- Decreased ear infections from resistant pneumococcus – this is considered a much more valuable benefit from the shot. The vaccine has been shown to significantly decrease the number of ear infections caused by pneumococcus that are resistant to standard antibiotics.
- Ear tubes.
These are tiny tubes that an
ENT specialist inserts into the eardrum under
general anesthesia. They usually stay in place for 6
months to over a year. There are several purposes
achieved by tubes:
- To drain chronic ear fluid that may turn into "glue ear".
- To provide an outlet for middle ear fluid to drain out as it begins to collect during a cold. This may help prevent a full ear infection from occurring.
- To preserve hearing and timely speech development by avoiding long months of muffled hearing caused by middle ear fluid.
- To help prevent the rare complication of chronic hearing loss caused by recurrent ear infections.
THE EAR TUBE CONTROVERSY
While ear tubes do have their place in treating recurrent ear infections, there does exist some controversy over their use. The advantages are listed above. Some common concerns about tubes are:
- Some doctors may be too quick to recommend ear tubes before exhausting all other preventative measures or before allowing enough time to allow the ears to clear up without surgery.
- As with any surgery, there are risks (though minimal) to general anesthesia.
- The tubes often leave a little scar covering approximately one sixth of the eardrum. This scar is often permanent. There does not seem to be any long-term consequence of this scarring, but we're not completely sure. Please note that recurrent ear infections with or without eardrum rupture can also lead to scarring.
- Please note that ear tubes don't always prevent ear infections. Some children will still get as many infections even with the tubes in, but the fluid drains out right away.
OVERALL EAR TUBES DO HAVE A PROPER PLACE IN TREATING RECURRENT EAR INFECTIONS WHEN USED APPROPRIATELY.
- Many children benefit from ear tubes. Parents declare their child is a new person. The ear infections are gone. The hearing is improved. No more sleepless nights with a crying child. No more endless courses of antibiotics.
- General indication for tubes are chronic ear fluid for more than four to six months; or more than three ear infections in six months or more than five in one year. You and your doctor should decide together when it is the right time for ear tubes for your child.